Healthcare Trends in the US: Shaping the Future of Wellness in 2025
Related Articles: Healthcare Trends in the US: Shaping the Future of Wellness in 2025
Introduction
In this auspicious occasion, we are delighted to delve into the intriguing topic related to Healthcare Trends in the US: Shaping the Future of Wellness in 2025. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Healthcare Trends in the US: Shaping the Future of Wellness in 2025

The healthcare landscape in the United States is in constant flux, driven by technological advancements, evolving patient preferences, and a growing emphasis on preventative care and value-based models. As we approach 2025, several key trends are poised to reshape the industry, impacting both healthcare providers and consumers. This comprehensive analysis delves into these trends, examining their potential benefits and implications for the future of American healthcare.
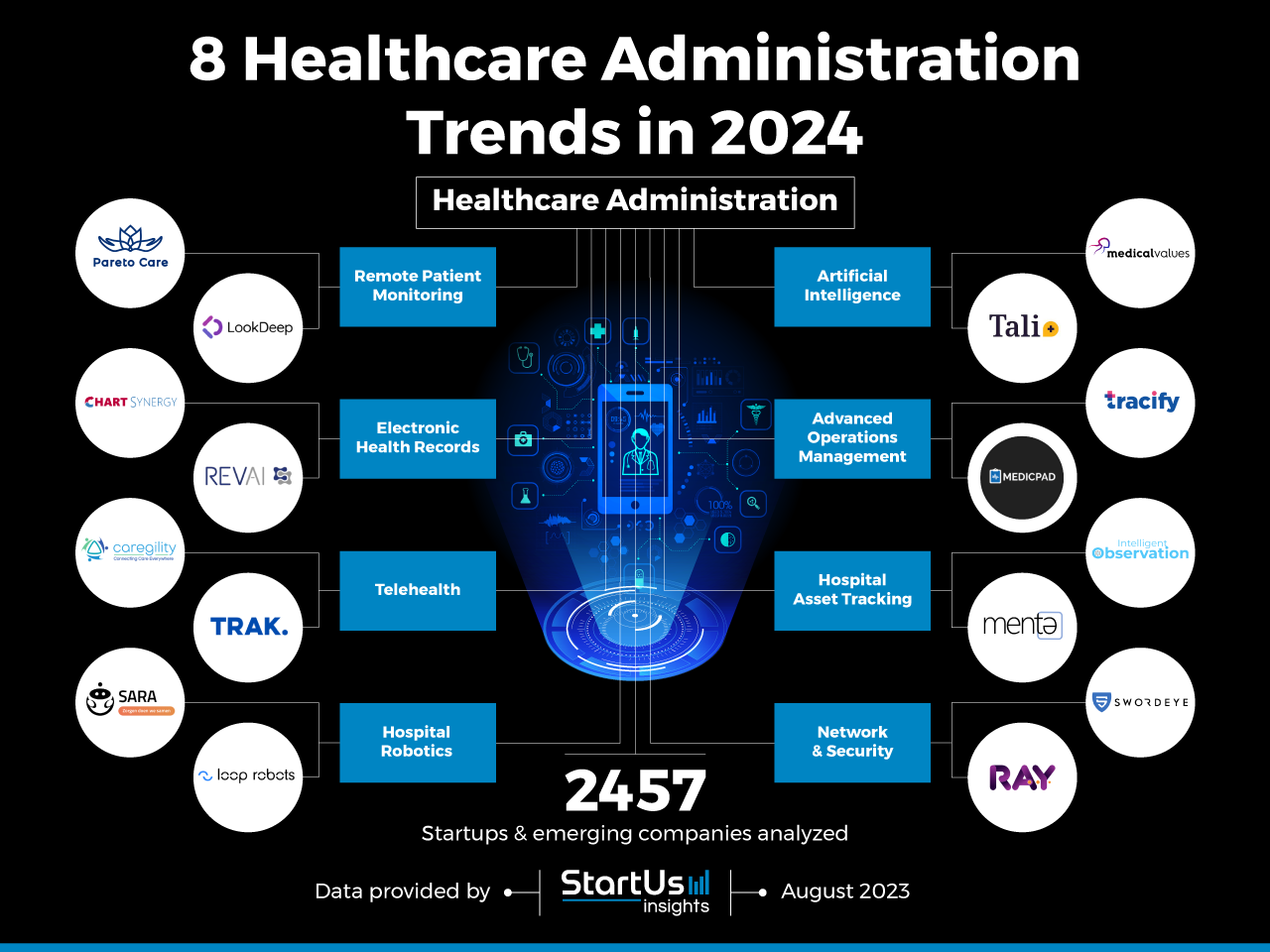
1. The Rise of Virtual Care and Telehealth
The COVID-19 pandemic accelerated the adoption of virtual care and telehealth services, transforming the way healthcare is delivered. This trend is projected to continue, with virtual consultations, remote monitoring, and online prescription refills becoming increasingly commonplace.
-
Benefits:
- Increased Accessibility: Virtual care removes geographical barriers, making healthcare services more accessible to individuals in rural areas or those with mobility limitations.
- Convenience: Patients can schedule appointments and receive care from the comfort of their homes, saving time and reducing travel costs.
- Improved Efficiency: Virtual care platforms streamline administrative processes, leading to shorter wait times and faster access to care.
- Cost Reduction: Telehealth can potentially reduce overall healthcare costs by minimizing hospital admissions and unnecessary in-person visits.
-
Implications:
- Integration of Technology: Healthcare providers need to invest in robust telemedicine platforms and ensure their staff is adequately trained in virtual care delivery.
- Data Security and Privacy: Strict protocols for data protection and patient privacy must be implemented to safeguard sensitive medical information.
- Regulatory Framework: Clear regulatory frameworks need to be established to govern telehealth practices and ensure patient safety and quality of care.
2. Personalized Medicine and Precision Healthcare
Personalized medicine, also known as precision healthcare, focuses on tailoring treatments to individual patients based on their unique genetic makeup, lifestyle, and environmental factors. This approach aims to optimize treatment effectiveness and minimize side effects.
-
Benefits:
- Targeted Therapies: Personalized medicine allows for the development of treatments that are specifically tailored to the patient’s individual needs, increasing the likelihood of successful outcomes.
- Reduced Adverse Effects: By understanding a patient’s genetic predispositions, healthcare providers can better predict and prevent potential side effects from medications or treatments.
- Proactive Health Management: Personalized medicine empowers individuals to take a more proactive approach to their health, making informed decisions based on their genetic risk factors.
-
Implications:
- Genomic Sequencing: The widespread adoption of genomic sequencing will require advancements in data analysis and interpretation, as well as ethical considerations regarding data privacy and potential discrimination.
- Collaboration and Data Sharing: Effective implementation of personalized medicine requires seamless data sharing between healthcare providers, researchers, and pharmaceutical companies.
- Investment in Research: Continued investment in research and development is crucial to unlock the full potential of personalized medicine and develop new, targeted therapies.
3. Artificial Intelligence (AI) and Machine Learning (ML) in Healthcare
AI and ML are transforming healthcare by automating tasks, improving diagnosis accuracy, and enabling data-driven decision-making. These technologies are being used in various applications, including medical imaging analysis, disease prediction, and drug discovery.
-
Benefits:
- Enhanced Diagnostic Accuracy: AI-powered tools can analyze medical images and patient data to identify patterns and anomalies that may be missed by human eyes, leading to earlier and more accurate diagnoses.
- Personalized Treatment Recommendations: AI algorithms can analyze patient data to predict the most effective treatment options based on individual characteristics and medical history.
- Improved Efficiency: AI can automate repetitive tasks such as scheduling appointments, processing claims, and generating reports, freeing up healthcare professionals to focus on patient care.
-
Implications:
- Ethical Considerations: The use of AI in healthcare raises ethical concerns regarding data privacy, algorithmic bias, and potential job displacement.
- Transparency and Explainability: AI systems need to be transparent and explainable, allowing healthcare providers to understand how decisions are made and ensuring patient trust.
- Data Infrastructure: The successful implementation of AI in healthcare requires robust data infrastructure, including secure data storage, efficient data processing, and standardized data formats.
4. Focus on Value-Based Care
Value-based care models shift the focus from volume-based healthcare to quality and outcomes. This approach incentivizes providers to deliver high-quality care while managing costs effectively.
-
Benefits:
- Improved Patient Outcomes: Value-based care encourages providers to prioritize patient health and well-being, leading to better overall outcomes.
- Cost Containment: By focusing on efficiency and preventing unnecessary procedures, value-based care models help control healthcare spending.
- Enhanced Care Coordination: Value-based care promotes better communication and collaboration among healthcare providers, ensuring a seamless patient experience.
-
Implications:
- Data Measurement and Reporting: Accurate data collection and reporting are essential for monitoring and evaluating the effectiveness of value-based care programs.
- Provider Incentives and Payment Models: New payment models need to be developed that reward providers for delivering high-quality care and achieving positive patient outcomes.
- Patient Engagement: Value-based care requires active patient participation in their health management, including adherence to treatment plans and lifestyle modifications.
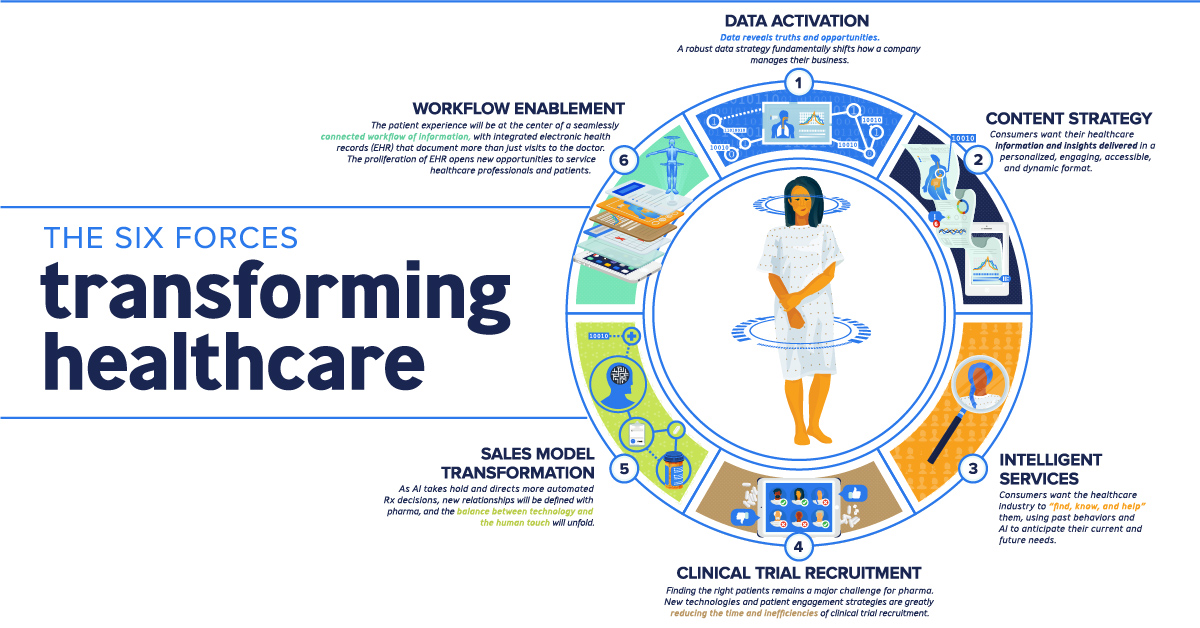
5. Consumer-Centric Healthcare
The healthcare industry is witnessing a growing trend towards consumer-centricity, with patients demanding greater control over their healthcare choices. This shift is driven by increased access to information, rising consumer expectations, and a desire for personalized care.
-
Benefits:
- Empowered Patients: Consumers are becoming more informed about their health conditions and treatment options, enabling them to make more informed decisions.
- Improved Patient Satisfaction: Healthcare providers that prioritize patient experience and cater to individual preferences are likely to see higher patient satisfaction rates.
- Increased Transparency: Consumers are demanding greater transparency from healthcare providers, including pricing information, quality metrics, and treatment outcomes.
-
Implications:
- Digital Health Tools: Healthcare providers need to leverage digital health tools and platforms to engage patients, provide personalized information, and facilitate communication.
- Patient Education and Engagement: Investing in patient education programs and tools can empower consumers to actively participate in their health management.
- Focus on Patient Experience: Healthcare providers need to prioritize the patient experience, ensuring a comfortable and supportive environment.
6. The Role of Genomics and Personalized Medicine in Disease Prevention
Genomics plays a crucial role in disease prevention by identifying genetic risk factors and enabling proactive interventions. Personalized medicine empowers individuals to make informed decisions based on their unique genetic predispositions.
-
Benefits:
- Early Detection: Genomic testing can identify individuals at higher risk for certain diseases, allowing for early interventions and potentially preventing disease progression.
- Lifestyle Modifications: Understanding genetic predispositions can motivate individuals to adopt healthier lifestyles, reducing their risk of developing certain conditions.
- Targeted Screening: Personalized medicine enables tailored screening programs based on individual risk factors, ensuring resources are used effectively.
-
Implications:
- Ethical Considerations: Genomic testing raises ethical concerns regarding data privacy, genetic discrimination, and the potential for over-diagnosis and unnecessary interventions.
- Accessibility and Cost: Genomic testing needs to be made accessible and affordable to ensure equitable access to preventative care.
- Education and Counseling: Individuals undergoing genomic testing require adequate education and counseling to understand their results and make informed decisions.
7. The Impact of Wearable Technology and Remote Monitoring
Wearable technology and remote monitoring devices are revolutionizing healthcare by providing continuous data on patient health and allowing for proactive intervention.
-
Benefits:
- Real-Time Data: Wearable devices collect real-time data on vital signs, activity levels, and sleep patterns, providing valuable insights into patient health.
- Early Detection: Remote monitoring allows for the early detection of health changes, enabling timely interventions and potentially preventing serious complications.
- Improved Patient Engagement: Wearable technology can motivate individuals to take a more active role in managing their health by providing personalized feedback and tracking progress.
-
Implications:
- Data Security and Privacy: Strict protocols for data security and privacy are essential to protect sensitive health information collected by wearable devices.
- Integration with Electronic Health Records: Seamless integration of wearable data with electronic health records (EHRs) is crucial for effective clinical decision-making.
- Regulatory Framework: Clear regulatory frameworks need to be established to govern the use of wearable technology in healthcare and ensure patient safety.
8. The Rise of Healthcare Consumerism
Healthcare consumerism refers to the growing trend of patients taking a more active role in their healthcare decisions, driven by factors such as increased access to information, rising healthcare costs, and a desire for personalized care.
-
Benefits:
- Empowered Patients: Consumers are becoming more informed about their health conditions, treatment options, and healthcare costs, enabling them to make more informed decisions.
- Increased Transparency: Healthcare providers are facing pressure to be more transparent about their pricing, quality metrics, and treatment outcomes, leading to greater accountability.
- Improved Patient Satisfaction: Healthcare providers that prioritize patient experience and cater to individual preferences are likely to see higher patient satisfaction rates.
-
Implications:
- Digital Health Tools: Healthcare providers need to leverage digital health tools and platforms to engage patients, provide personalized information, and facilitate communication.
- Patient Education and Engagement: Investing in patient education programs and tools can empower consumers to actively participate in their health management.
- Focus on Patient Experience: Healthcare providers need to prioritize the patient experience, ensuring a comfortable and supportive environment.
Related Searches:
- Healthcare Technology Trends in 2025
- Future of Healthcare in the US
- Healthcare Innovations in 2025
- Digital Health Trends in 2025
- Trends in Telehealth
- Artificial Intelligence in Healthcare
- Value-Based Care Models
- Personalized Medicine and Precision Healthcare
FAQs:
Q: How will these trends impact the cost of healthcare in the US?
A: The trends discussed above have the potential to both increase and decrease healthcare costs. While technologies like AI and telehealth can potentially reduce administrative costs and improve efficiency, personalized medicine and genomics-based interventions can be expensive. Value-based care models aim to control costs by incentivizing providers to deliver high-quality care while managing spending effectively.
Q: What are the ethical considerations surrounding these trends?
A: Many of these trends raise ethical concerns, including data privacy, algorithmic bias, genetic discrimination, and the potential for over-diagnosis and unnecessary interventions. It is crucial to establish clear ethical guidelines and regulatory frameworks to ensure responsible and equitable use of these technologies.
Q: How can healthcare providers prepare for these trends?
A: Healthcare providers need to invest in technology, training, and data infrastructure to support these trends. They should also prioritize patient engagement, transparency, and ethical considerations.
Tips:
- Embrace Technology: Healthcare providers should invest in digital health tools, telemedicine platforms, and AI-powered solutions to enhance care delivery and patient engagement.
- Prioritize Patient Experience: Focus on creating a comfortable and supportive environment, providing personalized care, and fostering open communication with patients.
- Invest in Data Infrastructure: Develop robust data infrastructure for secure data storage, efficient processing, and standardized data formats to support AI, personalized medicine, and value-based care models.
- Promote Patient Education: Invest in patient education programs to empower individuals to take a more active role in their health management and make informed decisions.
- Stay Informed: Continuously monitor industry trends and advancements to stay ahead of the curve and adapt to the evolving healthcare landscape.
Conclusion:
The healthcare trends discussed above are poised to reshape the industry in the coming years, creating opportunities for innovation, improved patient outcomes, and greater access to care. By embracing these trends, healthcare providers, policymakers, and consumers can work together to build a more efficient, effective, and equitable healthcare system for the future. However, it is essential to address the ethical considerations and potential challenges associated with these advancements to ensure responsible and equitable implementation.



Closure
Thus, we hope this article has provided valuable insights into Healthcare Trends in the US: Shaping the Future of Wellness in 2025. We thank you for taking the time to read this article. See you in our next article!